The main actions of Ozempic and GLP-1 drugs are to stimulate insulin secretion (i.e., to act as an incretin hormone) and to inhibit glucagon secretion, thereby contributing to controlling type 2 diabetes. An Economist podcast Babbage, explores the prospect for GLP-1 drugs being used in a whole range of new anti-inflammatory treatments including heart disease, liver disease, kidney disease, mental health treatment, Parkinsons Disease and dementia.
What Are GLP-1 Agonist Drugs
GLP-1 agonists are medications that help lower blood sugar levels and promote weight loss, and a number of them are available on the US market.
- Dulaglutide (Trulicity®).
- Exenatide (Byetta®).
- Exenatide extended-release (Bydureon®).
- Liraglutide (Victoza®).
- Lixisenatide (Adlyxin®).
- Semaglutide injection (Ozempic®).
- Semaglutide tablets (Rybelsus®).
There’s also a similar class of medications called dual GLP-1/GIP receptor agonists. There’s currently one of these medications on the market called tirzepatide (Mounjaro®).
Other names for this medication class include:
- Glucagon-like peptide-1 agonists.
- GLP-1 receptor agonists.
- Incretin mimetics.
- GLP-1 analogs.
How Do GLP-1 Drugs Work
When we eat, our gut sends out a large number of messages to help with the assimilation of nutrients and control how our food moves along our stomach and ultimately signals that we’re full. And one of these messages is a hormone, a small protein called GLP-1. It’s made at very low levels when we sleep or in the fasting state. But when we eat, its levels rise several times and it helps us dispose of the glucose. It also tells the pancreas to make insulin, and controls the rate at which our stomach empties. As well, it also signals to our brain that maybe we’ve had enough to eat and maybe we feel full. When there is inflammation due to the gut bacteria, it can rise much more.
GLP-1 agonist medications work by mimicking the natural hormone. In medication terms, an agonist is a manufactured substance that attaches to a cell receptor and causes the same action as the naturally occurring substance.
{This section copied from the Cleveland Clinic. }
- Triggers insulin release from your pancreas.
- Insulin is an essential hormone that allows your body to use the food you eat for energy. It lowers the amount of glucose (sugar) in your blood. If you don’t have enough insulin, your blood sugar increases, leading to diabetes.
- Blocking glucagon secretion:
- Glucagon is a hormone your body uses to raise your blood sugar levels when necessary. So, GLP-1 prevents more glucose from going into your bloodstream.
- Slowing stomach emptying:
- Slower digestion means that your body releases less glucose (sugar) from the food you eat into your bloodstream.
- Increasing how full you feel after eating (satiety):
- GLP-1 affects areas of your brain that process hunger and satiety.
Ozempic and GLP-1 Drugs Detail
Expanded Use of GLP-1 Antogist
Dr Caroline Messer, an endocrinologist is interviewed by the Economist Podcast and says that the anti-inflammatory action of GLP-1s has promise in the following areas. These are off-label but some are undergoing research trials. What she noticed was patients who had been put onto GLP-1 medication had benefits independent of the weight loss benefits (about 10-15% body weight loss).

- Decreased risk of cardiac incidents – lower heart attack, strokes (already approved) with improved heart health. Indicative improvement of more than 20%
- Reduction in autoimmune diseases such as IBS and rheumatoid arthritis
- Improved mental health
- Improved cognitive skills
- Reduced polycystic ovary syndrome – with restoration of fertility.
- Reduced diarrhoea due to irritable bowel syndrome.
- Reduced sleep apnoea.
- Kidney function improvement
- Less fat on the liver
- Reduced binge eating disorders where nothing else had helped.
- Decreased propensity to drink – enabling drink moderately.
- Patients with early cognitive impairment.
Wide-Ranging Benefits of GLP-1
Messer stated there may be a very low threshold for prescribing it for other issues in the appropriate patients.
The Economist also interviewed Prof Daniel Drucker of the University of Toronto and Mount Sinai Hospital, confirming that these benefits appear real, based on observations, initial clinical studies and animal studies.
Improvement in Heart Disease
There are GLP-1 receptors on blood vessels and heart cells. Medicines that help control some of the blood lipids and blood pressure also reduce inflammation. These GLP-1 medications reduce blood lipids, reduce blood pressure and provide weight loss. All of these measures can help reduce the rates of heart disease. The researchers think there may be some direct effects on the blood vessels on the heart, which show a reduction in strokes and heart attacks seen in people treated with these GLP-1. Inflammation is a powerful driver for the development of atherosclerosis and blood vessel disease and makes heart attacks more likely.
Protects Cell Health – Liver and Kidney
Beyond the benefits of losing weight and having better blood sugar control, GLP-1 protects the health of cells. If you have GLPT-1 receptors on your cells and are vulnerable, having GLP-1 on board seems to allow the cells to be maintained in a healthier state and less susceptible to death. Inflammation is a powerful driver of all the diseases. Given GLP-1 reduces inflammation in many parts of the body, it likely contributes to some of the benefits.
Regulatory approval is likely within the next 2 years for kidney and liver benefits.
Mental Impacts
People who are drinking alcohol, smoking cigarettes, using narcotics or cannabinoids, or have dependence-related behaviours, including increased shopping and excessive consumption of foods. GLP-1 appears to control our reaction to these pleasurable behaviours. One explanation may be related to modulating the pleasure signal dopamine. Other pathways are still being explored. Trials underway are seeing whether some of these checkpoint medicines can be repurposed to help people with these dependence disorders. Drucker pointed out that imaging can show people’s brains and show how they react to pleasurable substances in the absence or presence of children.
Neurological and Dementia
Preliminary evidence suggests potential benefits in autoimmune diseases with observed reductions in inflammation markers, but this is mainly based on observational data and requires more controlled trials for validation.
There is potential for reducing dementia risk, yet supporting clinical data are insufficiently established, and will need further studies.
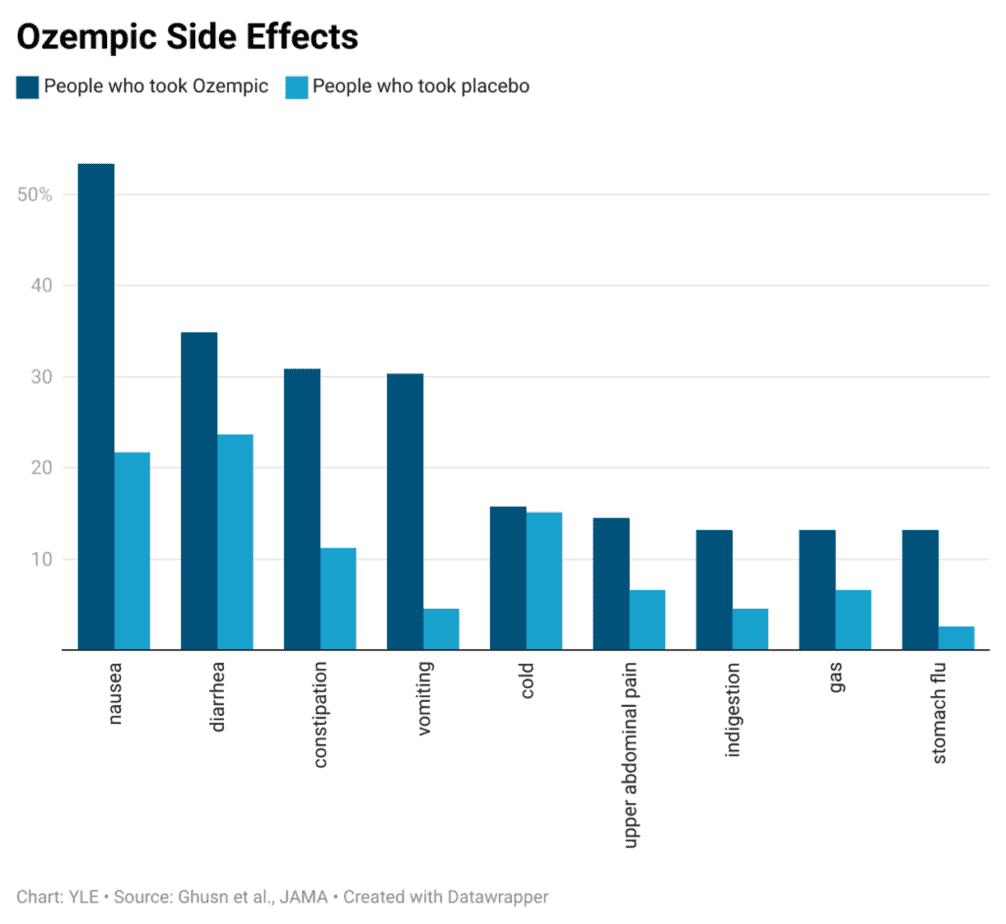
Risks
There are some concerns about thyroid cancers. Some have nausea, and some do not appear to tolerate the drugs. Specified side effects include
- inflammation of your pancreas (pancreatitis).
- changes in vision.
- low blood sugar (hypoglycemia). …
- kidney problems (kidney failure).
- serious allergic reactions.
- gallbladder problems.
Some has said there is muscle loss, but that is normal with most diets. If you stopping taking the drugs, you put that weight back on – for most people, just like any other weight loss program.
Costs
Costs can be up to $935 per month or $11,000 per year without a prescription in the USA. In Australia, where the drug is on the PBS, people with diabetes can get a three-week supply for A$31.60 ($7.70 for concession card holders) rather than the full price ($133.80). That is an annual cost of $AU2,300 per year.
Most of the patents do not expire until 2032 to 2036 in the USA, but in countries like China, India, and Brazil some GLP-1 drugs will come off patent as early as 2026.
Formulation into capsules from the injectable form or other formulations will reduce cost and improve availability.
New Drugs
In the 1960s, researchers showed the incretin effect was responsible for about two-thirds of people’s insulin response. New and sensitive ways to measure blood hormone levels then allowed researchers to show a hormone called GIP (glucose‐dependent insulinotropic polypeptide) was partly responsible for the incretin effect.
Glucagon is another hormone that your pancreas makes to help regulate blood glucose (sugar) levels. Glucagon increases your blood sugar level and prevents it from dropping too low, whereas insulin decreases blood sugar levels.
So now the chemists and drug companies have 3 targets. GLP-1, glucagon, and GIP.
A combination of GLP-1, GIP, and glucagon may increase weight loss to up to 24%. Eli Lilly is now in mid-stage clinical trials with retatrutide (once-weekly injection).
This won’t be the last.
References
- How could Ozempic and its cousins change health care? Babbage The Economist Podcast Oct 2024 https://www.economist.com/podcasts/2024/10/30/how-could-ozempic-and-its-cousins-change-health-care
- GLP-1 Agonists 2024 https://my.clevelandclinic.org/health/treatments/13901-glp-1-agonistshttps://my.clevelandclinic.org/health/treatments/13901-glp-1-agonists
- Considering taking a weight-loss drug like Ozempic? Here are some potential risks and benefits? https://public-health.uq.edu.au/article/2024/04/considering-taking-weight-loss-drug-ozempic-here-are-some-potential-risks-and-benefits
- Here’s How Much More Ozempic Costs in the U.S. Compared to Other Countries https://www.healthline.com/health-news/heres-how-much-more-ozempic-costs-in-the-u-s-compared-to-other-countries
- Weight-loss: Are injections the answer to tackling obesity? 2023 https://www.bbc.com/news/health-64677915
- The rise of Ozempic: how surprise discoveries and lizard venom led to a new class of weight-loss drugs April 2024 https://theconversation.com/the-rise-of-ozempic-how-surprise-discoveries-and-lizard-venom-led-to-a-new-class-of-weight-loss-drugs-219721