Recent evidence shows statin effectiveness in older people aged 60 to 75 moderately reduces ischemic stroke risk, but consistent benefit beyond age 75 is unclear, and significant gaps remain in stroke-specific, standalone data for older adults [1] [2] [3].
Statins, Elevated Cholesterol and Strokes
Stroke remains a significant cause of morbidity and mortality worldwide, with older adults, particularly those over age 60, at the highest risk of first-time ischemic stroke. Statins, or HMG-CoA reductase inhibitors, are widely prescribed for cardiovascular disease (CVD) prevention due to their proven efficacy in lowering low-density lipoprotein cholesterol (LDL-C) levels, stabilizing atherosclerotic plaques, and reducing inflammation. There are 2 cases: primary and secondary.
Primary – Never had an Event
Evidence for their effectiveness in primary prevention, specifically focused on stroke, is less robust, particularly in elderly populations. This is especially true for those over age 75, where guideline recommendations remain inconsistent due to data gaps [1] [4] [5].
Secondary – Followup after an Event
Statins help reduce any following events if you have already had an event (CVD, stroke). So if you survive the first event, take statins.
If you want to assess your personal risk (and not these population risks) check out the baseline risk of cardiovascular disease estimated such as the online calculator QRisk.
Effectiveness of Taking Statins in Younger People
There has been an ongoing debate about whether or not statins are over-prescribed. Does everyone who takes them really benefit from them? One has to look at absolute risk versus relative risk.
Imagine your chance of dying from a certain condition prematurely is 0.2%, and there’s a drug that reduces your chance of dying to 0.1%. In relative terms (relative risk reduction), your chance of dying has been halved, or reduced by 50%. But in absolute terms (absolute risk reduction), your chance of dying has only gone down by 0.1%.
The conclusion from a meta analysis of 140,000 people in 21 studies was the absolute risk reduction from taking statins was modest compared with the relative risk reduction in absolute terms.
A man would reduce his risk from 38% to 34.6%, and the woman from 1.4% to 1.3% [11] says Paula Brown..
| Indicator | Relative Risk | Absolute Risk |
|---|---|---|
| Deaths | 9% | 0.8% |
| Heart Attacks | 29% | 1.3% |
| Strokes | 14% | 0.4% |
| Having any event | Male 38% down to 35% Female from 1.4% to 1.3% |
If you have had a CVD event, and survived, then statins have an unequivocal benefit in reducing CVD risk across age groups for secondary prevention. For those receiving statins for 5 years and attaining a 1 mmol/L reduction in LDL cholesterol, this equates to absolute risk reductions in those with intermediate risk of 4 vascular deaths saved per 1000 and 15 vascular events per 1000.
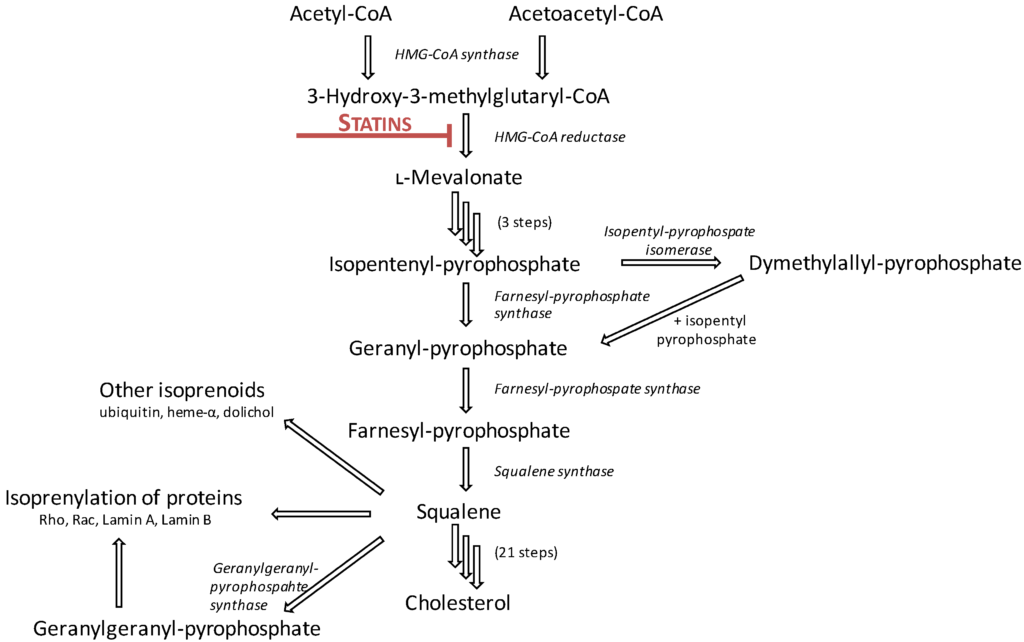
Mechanism of Statins
Statins are competitive inhibitors of 3-hydroxy-3-methylglutaric coenzyme A (HMGCoA), a key enzyme in the biosynthesis of cholesterol that converts HMGCoA to mevalonate. This reduces the amount of cholesterol. But this process also interferes with other biochemical processes. Cholesterol is needed as a building block for a range of other normal functions – they are precursors to chemicals.
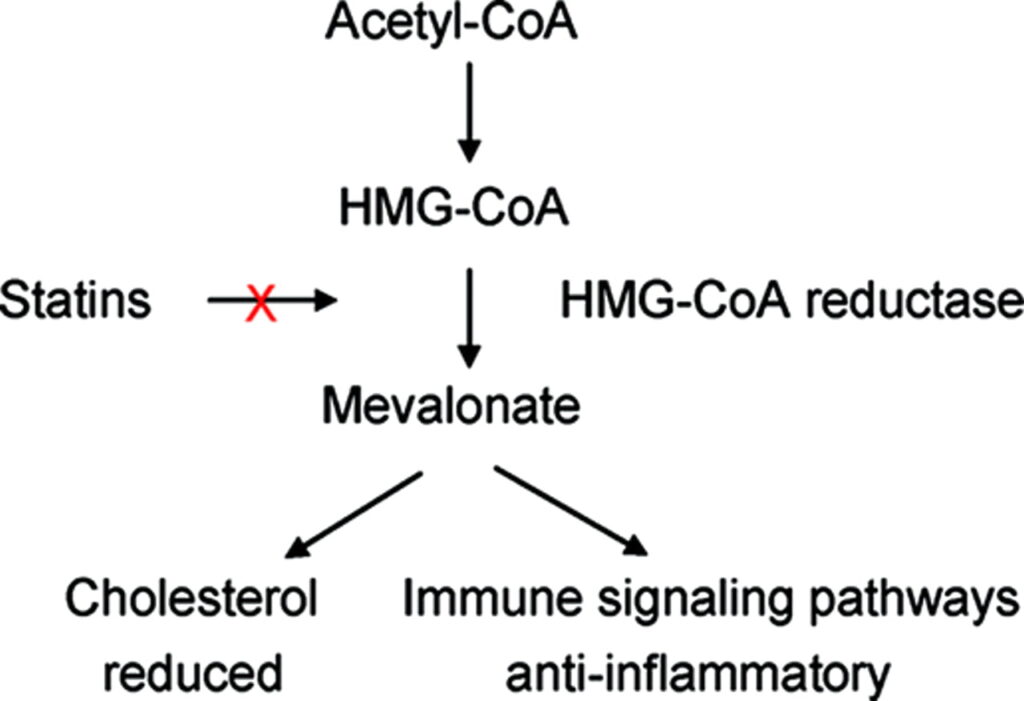
Generally, the benefit from the reduction of cholesterol, and in particular LDL-C provides much of the benefit, but we also know it has anti-inflamatory properties because some of the inflammation markers are reduced.
What’s the Evidence for Statin Effectiveness in Older People?
Scientists are trying to clarify the role of statins in reducing stroke events among older adults in a primary prevention setting. Systematic reviews and meta-analyses, such as those conducted by Huang [1] and Zhai [6], aggregate existing data from trials and observational studies. Huang [1]demonstrated a moderate reduction in stroke and cardiovascular mortality in individuals aged 65 and older, although most included studies did not isolate stroke-specific outcomes from composite cardiovascular endpoints. Similarly, Zhai et al. [6] showed a significant reduction in cardiovascular events with statins in elderly patients, but stroke-specific benefits in primary prevention settings were not robust.
Age-specific considerations are critical in interpreting these findings. While meta-analyses indicate a modest benefit for individuals aged 60–75 years, reviews such as those by Nanna et al. [7] and Rasmussen et al. [8] emphasize that uncertainty increases for adults over 75 years, where randomized controlled trial (RCT) data are sparse or contradictory. Indeed, studies like ALLHAT-LLT ,[9] which analyzed statins in older adults without established CVD, reported inconclusive results for stroke prevention. This lack of clarity has prompted ongoing trials such as STAREE and PREVENTABLE to directly address primary prevention outcomes in individuals over age 75, though results are not yet available [7], [10]].
Several challenges further complicate the interpretation of these studies.
- Composite endpoints, common in cardiovascular studies, often dilute stroke-specific outcomes and make it difficult to isolate the standalone impact of statins on stroke risk.
- Concerns regarding hemorrhagic stroke, while rare, linger in elderly populations, particularly in those with very low LDL-C levels or vulnerable cerebrovascular conditions.
- Iindividualization of care, which considers factors such as frailty, competing risks, polypharmacy, and life expectancy, is essential for older adults, as highlighted by geriatric-focused reviews .
Further Work Needed.
We need to refine the understanding of statins’ standalone effectiveness in reducing first-time stroke events among individuals aged over 60. Data suggests a modest benefit in relatively younger elderly populations (60–75 years).
There is uncertainty for older adults, particularly those aged over 75.
Further evidence from ongoing trials is expected to address these knowledge gaps and inform clinical decision-making.
References
[1] “Statin use in older people primary prevention on cardiovascular disease: an updated systematic review and meta-analysis.” Accessed: Dec. 18, 2024. [Online]. Available: https://www.imrpress.com/journal/RCM/23/4/10.31083/j.rcm2304114/htm
[2] M. G. Varughese and C. M. Ballantyne, “The 2022 American College of Cardiology Expert Consensus on the Role of Nonstatin Therapies: An Expert-Guided Tour,” Tex. Heart Inst. J., vol. 50, no. 6, p. e238233, Nov. 2023, doi: 10.14503/THIJ-23-8233.
[3] G. Spencer-Bonilla, S. Chung, A. Sarraju, P. Heidenreich, L. Palaniappan, and F. Rodriguez, “Statin Use in Older Adults with Stable Atherosclerotic Cardiovascular Disease,” J. Am. Geriatr. Soc., vol. 69, no. 4, pp. 979–985, 2021, doi: 10.1111/jgs.16975.
[4] R. C. Shah, M. A. Supiano, and P. Greenland, “Aligning the 4Ms of Age-Friendly Health Systems With Statin Use for Primary Prevention,” J. Am. Geriatr. Soc., vol. 68, no. 3, pp. 463–464, 2020, doi: 10.1111/jgs.16325.
[5] “Statins for Primary Prevention in Older Adults: Uncertainty and the Need for More Evidence | Cardiology | JAMA | JAMA Network.” Accessed: Dec. 18, 2024. [Online]. Available: https://jamanetwork.com/journals/jama/article-abstract/2584059
[6] C. Zhai et al., “Efficacy of statin treatment based on cardiovascular outcomes in elderly patients: a standard meta-analysis and Bayesian network analysis,” J. Int. Med. Res., vol. 48, no. 6, p. 0300060520926349, Jun. 2020, doi: 10.1177/0300060520926349.
[7] “Current Opinion in Cardiology.” Accessed: Dec. 18, 2024. [Online]. Available: https://journals.lww.com/co-cardiology/abstract/2023/01000/primary_prevention_statin_therapy_in_older_adults.4.aspx
[8] P. Rasmussen, S. Yandrapalli, and W. Aronow, “Statin therapy for primary cardiovascular prevention in adults older than 75 years,” Pol. Heart J. Kardiologia Pol., vol. 79, no. 1, Art. no. 1, 2021, doi: 10.33963/KP.15743.
[9] “Effect of Statin Treatment vs Usual Care on Primary Cardiovascular Prevention Among Older Adults: The ALLHAT-LLT Randomized Clinical Trial | Cardiology | JAMA Internal Medicine | JAMA Network.” Accessed: Dec. 18, 2024. [Online]. Available: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2628971
[10] C. Heneghan and K. R. Mahtani, “Absolute effects of statins in the elderly,” BMJ Evid.-Based Med., vol. 24, no. 5, pp. 200–202, Oct. 2019, doi: 10.1136/bmjebm-2019-111189.
[11] “newsGP – Have the benefits of statins been overstated?,” NewsGP. Accessed: Dec. 19, 2024. [Online]. Available: https://www1.racgp.org.au/newsgp/clinical/have-the-benefits-of-statins-been-overstated
Not Medical Advice
This is not medical advice.
Go to your GP for advice
Checkout QRisk to make that assessment on risk personal









